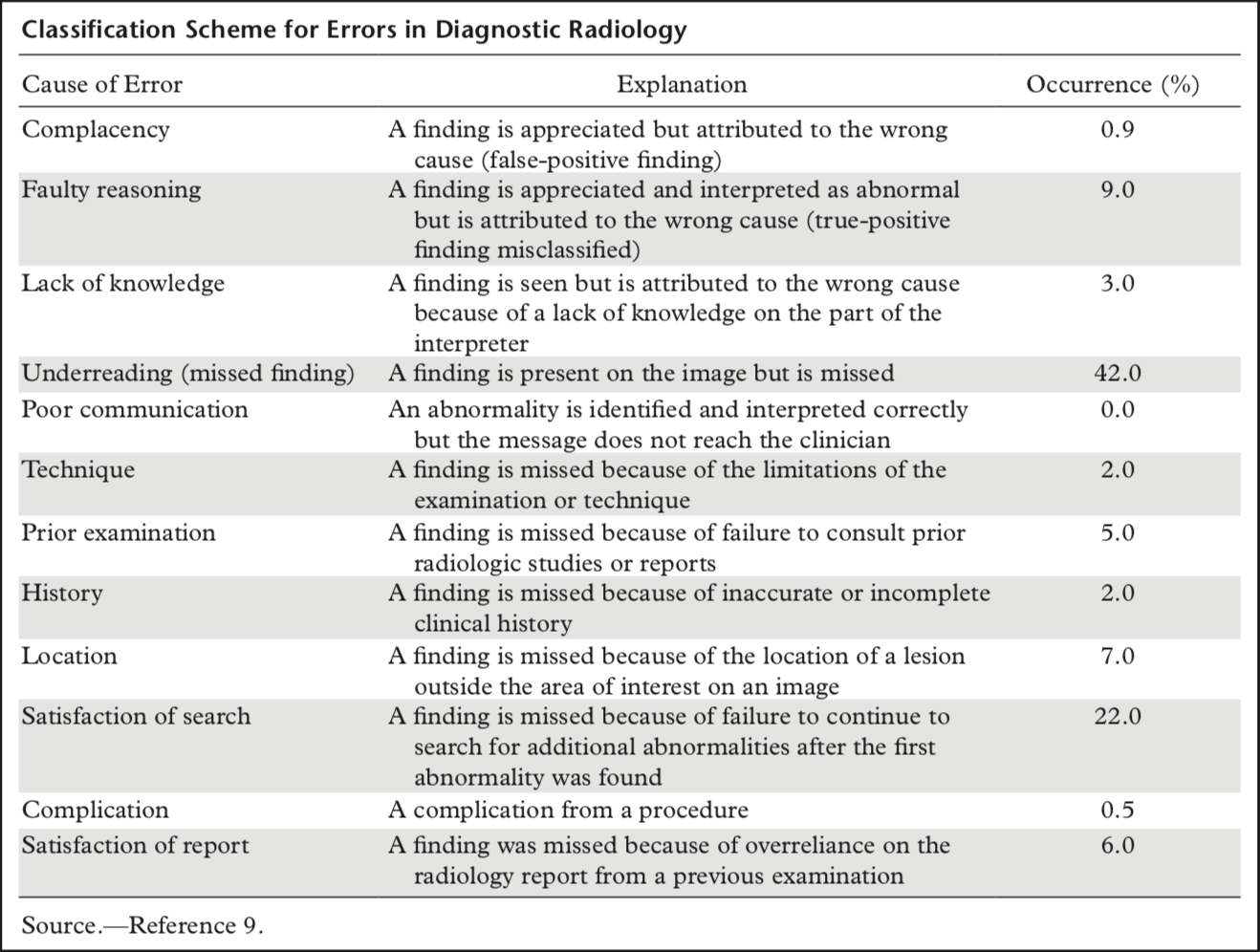
According to [Bruno et al. (2015)](https://pubs.rsna.org/doi/pdf/10.1148/rg.2015150023), the most common error in radiology is "underreading", i.e. simply overlooking findings. If you add up all the types of errors that result from overlooking a finding, these account for almost 90% of errors in radiology. Yet it is mostly the increase of knowledge and not the finding of findings that is talked about in the training of radiology residents.
The first thing I was told in my radiology internship was that I should think of a structure for looking at a chest X-ray. The exact structure and sequence didn't matter, as long as I always did it the same way. In retrospect, I disagree with this statement. Of course the order in which I look at the image doesn't matter. But the individual points I look at in an X-ray are do matter very much. And leaving these individual points to an inexperienced medical student or radiologist is wrong.
Experienced radiologists have a checklist in their head of things to look at. However, there are a few problems with this approach.
The checklist in your head is merely implicit, relying on you to concentrate so you don't skip an item on your checklist. As a radiologist, however, you are constantly disturbed. The phone is constantly ringing or the technician comes in and asks something. And immediately you are pulled out of your diagnostic work. There is a danger that you forget important points on your implicit checklist.
Moreover, this implicit checklist is individual for each radiologist. Every radiologist thinks up the points he looks at in an examination himself. This makes the report variable, depending on which radiologist has written them.
So how can these points be countered?
With an explicit checklist of things to look at in an examination.
This approach has several advantages:
Reports that are created based on a checklist have a uniform structure and are thus easier to compare with each other. In addition, a central list of things to look at to complete an examination leads to a consistent and potentially higher standard of findings.
A consistent structure also simplifies communication with referring colleagues. Clinicians know exactly what to expect when they request a certain examination and know exactly where to find the relevant information they need to treat their patients. In addition, having a centralised list of things to include in a report ensures that it contains all the things that are important to the clinician in deciding what to do with the patient. In this way, the report offers greater added value for both clinicians and patients.
In addition, young clinicians can be supported by a checklist during complex examinations. The lists can be created by experienced doctors and thus help to pass on experience to the young colleagues. This way, not every resident has to reinvent the wheel every time.
Additionally, a checklist leads to a more efficient use of the most important resource in the hospital: time. A list makes it easier to get back to the images after an interruption because you know exactly where you have to continue.
Tools like [Smart Reporting](https://smart-reporting.com/) or report templates like [radreport.org](http://radreport.org/) of the RSNA try to solve the problem similarly. Unfortunately, however, these have not yet become part of everyday life in many radiology departments. One reason may be that a tool like Smart Reporting has to be integrated very deeply into the existing IT infrastructure so that the previous workflow does not have to be changed.
Even if you still want to dictate your findings as free text, you can still use a checklist to ensure that the findings contain everything important and that you have looked at everything.
In any case, as radiologists we have to think about how we can maintain a high quality of our reports while simultaneously keeping the reporting process highly efficient. With the advent of AI we need to make sure that we maintain our central role in the clinical decision-making process.
## Further Reading
[The Checklist Manifesto by Atul Gawande](https://www.amazon.com/Checklist-Manifesto-How-Things-Right-ebook/dp/B0030V0PEW)